What is ICSI?
Intracytoplasmic sperm injection, known as ICSI, serves as a beacon of hope for many aspiring parents grappling with male infertility issues. While it falls under the wider umbrella of IVF, its uniqueness lies in its intricate procedure and specific purpose.
With traditional IVF, numerous sperm and an egg are combined in a petri dish, emulating the natural process of fertilization where the most capable sperm fertilizes the egg. ICSI, however, takes this process a step further. It involves the careful examination, selection, and injection of a single healthy sperm straight into the cytoplasm of an egg.
This precision bypasses any potential hindrance the sperm might face in reaching the egg, thus significantly enhancing the chance of fertilization. This becomes particularly crucial when the cause of infertility resides in sperm facing issues with motility or count, or having abnormal morphology.
Who is ICSI for?
ICSI, originally developed to treat severe male infertility, has nurtured countless dreams into reality. When the quandary lies in a low sperm count, poor sperm movement, or irregular sperm shape, ICSI emerges as a solution.
Additionally, where obstructions in the male partner’s reproductive tract prevent sperm from reaching the ejaculate or when previous IVF cycles have failed due to unexplained reasons, the process signifies a light at the end of the tunnel.
However, one fundamental aspect to remember when considering ICSI is that this intervention is not a one-size-fits-all solution. An infertility diagnosis is a complex puzzle, interlocking physical imbalances with, at times, genetic irregularities.
Consequently, an IVF specialist considering recommending ICSI to a couple does so only after a comprehensive evaluation and keeping in mind the individual circumstances surrounding their situation.
Success Rates and Statistics: The Efficacy of ICSI
Before embarking on any medical journey, it is wise to examine the roadmap of past voyagers – in this case, the success rates and associated statistics of ICSI. Statistics offer solace in numbers, an anchor of expectation in the fluid seas of fertility treatments.
ICSI boasts promising numbers: fertilization rates hover around 70-80%, markedly higher than the 50-60% attributed to conventional IVF. When considering clinical pregnancy rates, ICSI maintains a 40-50% success rate per embryo transfer cycle.
Furthermore, couples may experience a live birth rate of 30-40% per cycle, according to IVF success rate data. These figures easily brand ICSI as a favorable choice, especially in cases where severe male infertility is evident.
Nonetheless, it is paramount to harbor realistic expectations; these statistics, while encouraging, represent averages. Influential factors such as the age of the female partner, quality of the sperm and eggs provided, and the specific nuances of the couple’s infertility cause, all play crucial roles in determining success. Furthermore, the expertise of the clinic and embryologist conducting ICSI can be determinative.
It bears noting—multiple cycles may be necessary; success is seldom guaranteed on the first attempt. Acknowledging this can soften the blow of coping with IVF failures, should they occur, and foster resilience in subsequent cycles.
Ultimately, in making a decision as significant as this, remember that the average statistics serve as a general guide, not a crystal ball foreseeing individual outcomes. A detailed consultation with a fertility specialist is imperative to receive personalized success estimates tailored to your distinctive story.
The ICSI Journey: A Step-by-Step Encounter
Delving into the practicalities, the journey of ICSI is an odyssey of its own, composed of meticulous stages each lending itself to the next.
- Stimulation and Egg Retrieval:
This initial phase involves the administration of hormonal medications to the female partner, designed to stimulate the production of multiple eggs. The maturity of these eggs is diligently monitored through blood tests and ultrasounds, leading up to their retrieval via a transvaginal ultrasound-guided needle aspiration—a procedure requiring precision and delicacy.
- Sperm Preparation:
Concurrently, the male partner’s semen sample is meticulously analyzed in a quest to isolate healthy and viable sperm. In cases of severe male infertility, sperm may need to be retrieved directly from the testes or epididymis through procedures such as TESE or TESA.
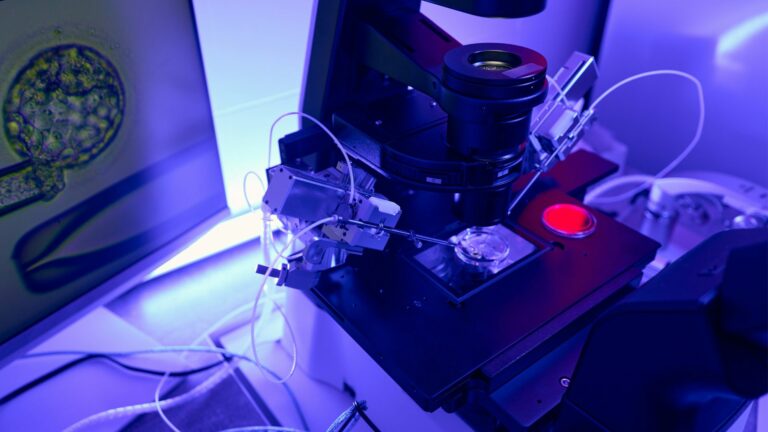
- Micromanipulation and Injection:
With eggs and sperm at their disposal, embryologists engage in micromanipulation—a delicate process necessitating profound skill and experience. A healthy, viable sperm is immobilized, then injected directly into the cytoplasm of an egg. This technique requires exceptional precision, as the embryologist must navigate the egg’s outer layers without compromising its integrity.
- Fertilization and Embryo Culture:
Post-injection, close surveillance is essential. The eggs are kept under watchful eyes and optimal conditions, poised to signal the early stages of life. Those that exhibit signs of fertilization begin their journey of cell division, marking the inception of embryonic development.
- Embryo Selection and Transfer:
As the incubated embryos mature, decisions loom on the horizon. Which to select for transfer? The choice hinges on thorough embryonic development assessments, performed by embryologists seeking to identify the most viable candidates for implantation.
After ICSI: Monitoring and Embryo Transfer
With the delicate process of ICSI complete, attention shifts to the critical phase of monitoring and the eventual transfer of embryos into the hopeful mother’s womb. This stage is as much about the science of growth as it is about the art of patience.
Monitoring Embryo Development
Post-fertilization, the embryology lab becomes a nursery where each embryo is tenderly nurtured and closely watched. This intricate dance of development is crucial:
- Cell division: Embryologists look for consistent division and growth, ensuring the embryo is developing as expected.
- Morphological development: The shape and form of the embryo at each stage give vital clues about its potential.
- Blastocyst formation: Reaching this stage is a significant milestone indicating that the embryo is likely ready for implantation.
During this time, couples might find themselves awash with anticipation and anxiety. This is normal, and finding support during the IVF process can be immensely beneficial for navigating these emotional waters.
Embryo Selection and Transfer
From a cohort of embryos, the embryologist along with the medical team will select the most viable ones for transfer. Leveraging years of experience and keen observation, one or sometimes two embryos will be gently transferred into the uterus—a moment that couples often recall with a blend of nerves and hope.
This critical juncture is guided by ultrasound, ensuring the optimal placement within the uterine lining. The procedure is typically painless and marks the final medical act of the ICSI journey. Patients typically resume normal activity shortly after, carrying with them the promise of new life.
Pregnancy Testing and Support
After the embryo transfer, the waiting begins. Roughly two weeks later, a pregnancy test can confirm whether implantation has occurred. This interval can be one of the most emotionally charged periods for couples.
Regardless of the outcome, the importance of emotional support cannot be understated—to buoy the spirits if results are not as hoped, or to share in joy if pregnancy is achieved. Understanding the psychological effects of IVF and being prepared for a variety of outcomes can help alleviate some of the stress associated with this waiting period.
Potential Risks and Side Effects
Every medical procedure, no matter how advanced, carries with it the weight of potential risks and side effects. ICSI is no exception. It’s important for couples to have a frank and transparent conversation about these possibilities with their doctor, to ensure a clear and comprehensive understanding of what may lie ahead.
Risks Associated with Egg Retrieval
The journey to retrieve eggs is not without its hazards, albeit minimal. Ovarian hyperstimulation syndrome (OHSS) is a rare but serious response to the hormonal drugs used to stimulate the ovaries. There can also be risks of bleeding or infection from the retrieval procedure itself. However, with an experienced team and careful monitoring, these risks are significantly minimized.
Risks Associated with the ICSI Procedure
The act of injecting a sperm into an egg is a feat of modern science, but the procedure is not infallible. There is a rare possibility of egg damage during the process, or a chance that fertilization may not occur. Multiple pregnancy is another consideration, as it is something that might be desired by some but comes with increased risks for both mother and babies.
General Risks and Side Effects
Beyond the procedure-specific risks, there are general concerns as well. These include the risk of miscarriage, which remains consistent with natural conception rates. Additionally, although advanced, the techniques involved with ICSI could conceivably increase the likelihood of certain types of birth defects, though overall, this risk is considered low.
Lastly, it’s impossible to overlook the emotional stress associated with the treatment, especially given the considerable investment of hopes, time, and resources.
Emotional and Psychological Support
Understanding the potential setbacks and managing one’s emotional health is as crucial as the physical aspects of ICSI. Couples are encouraged to seek support, whether through therapy, support groups, or through resources that help in coping with ICSI’s emotional impact.
Weighing the Options: The Benefits and Drawbacks of ICSI
When it comes to making a decision as significant as undergoing ICSI, it is beneficial to methodically weigh all the advantages and potential disadvantages. Couples equipped with comprehensive knowledge and transparent dialogue with their healthcare providers will traverse the emotional and ethical landscape of ICSI with greater confidence.
Benefits of Choosing ICSI
ICSI shines a ray of hope for couples facing harsh male infertility diagnoses by offering several distinct benefits:
- Enhanced Fertilization Rates: ICSI directly confronts sperm-related infertility issues by significantly improving fertilization outcomes, even in challenging conditions.
- Overcoming Male Infertility: Tailored to deal with low sperm counts, poor motility, abnormal morphology, or blockages, ICSI provides men an opportunity to father biological children.
- Alternative Sperm Retrieval: Techniques like TESE or TESA broaden the horizon for men who cannot produce sperm in their ejaculate, ensuring their genetic material can still create embryos.
- Increased Pregnancy Likelihood: The overall chances of achieving a successful pregnancy through ICSI exceed those of conventional solutions when factoring in severe male infertility.
Drawbacks to Consider
Amidst the optimism, realities must be acknowledged:
- Emotional Strain: The emotional gravity enveloping ICSI arises not just from the procedure’s complexity but also from the high stakes of its outcome, demanding robust emotional resilience.
- Financial Considerations: Financial aspects, particularly when considering ICSI’s cost relative to traditional IVF, can be substantial, and not all insurance plans offer comprehensive coverage.
- Ethical and Moral Considerations: For some couples, the interventionist nature of ICSI might stir ethical debates or clash with personal beliefs about the start of life and reproductive assistance.
Making an Informed Decision about ICSI
Couples must consult with their fertility specialist, address all concerns, and deliberate on the paths available to them, considering not only the potential for a successful outcome but the emotional journey associated with ICSI.
Fostering a robust support system, gaining insights from others’ experiences, and acknowledging the spectrum of outcomes can poise couples to face their fertility journeys with grace and informed readiness.
Making an Informed Decision about ICSI
Embarking on the ICSI journey demands more than just an understanding of the medical procedure; it requires a holistic approach that considers every facet of a couple’s life. Navigating these waters is not just a clinical endeavor—it is deeply personal, profoundly intimate, and requires a decision shaped not only by facts but also by feelings and future aspirations.
Individual Circumstances and Diagnosis
At the heart of the decision to pursue ICSI is a unique and individual story. Each couple brings their own set of circumstances, medical histories, and personal dreams to the table.
This diversity means that there is no one-size-fits-all answer; the decision to undergo ICSI must be tailored to the specific nuances of each case, guided by a thorough diagnosis and mutual agreement on the desired path forward.
Success Rates, Expectations, and Emotional Considerations
While success rates offer a beacon of hope, it’s the management of expectations that steers the emotional journey. Understanding and accepting the variables at play—including the unpredictability of the treatment’s outcome—helps brace couples for all possible futures. Investing in emotional resources and support systems before embarking on ICSI can provide much-needed solace, regardless of the result.
Financial Implications and Ethical Considerations
Financial readiness is another cornerstone of the ICSI decision. With costs potentially placing a significant burden on couples, understanding how to navigate these challenges—perhaps through resources on managing IVF on a budget—is crucial.
Moreover, each couple must align with ICSI ethically, examining their own values concerning reproductive technologies and the implications of creating life through these means.
Support, Communication, and the Value of a Strong Partnership
Central to the ICSI journey is a strong partnership and the power of communication—not just with each other, but with the team of healthcare providers. Finding a reproductive endocrinologist with whom couples feel comfortable discussing their concerns and who can provide clear, empathetic guidance is invaluable.
Empowerment through Information and Self-Advocacy
Ultimately, making an informed decision about ICSI is about empowerment. It’s about equipping oneself with knowledge, asking the right questions, understanding the steps to potentially increase IVF success, and advocating for one’s own needs and desires throughout the fertility journey.
Conclusion
As we conclude this guide to ICSI, remember: the path to making an informed decision is unique to each couple and should be traversed with care, consultation, and comprehensive consideration of all facets—medical, emotional, financial, and ethical. With a wealth of resources available, from scientific data to shared experiences and support, the journey of ICSI, while multifaceted, need not be navigated alone.
For those facing the complexity of male infertility, ICSI offers a route filled with promise and potential. By engaging in diligent research, sustained dialogue with professionals, and deep introspection, couples can approach this path not merely as passengers but as informed navigators of their own destiny.