The two pink lines on a pregnancy test—a symbol of hope, a dream coming true. For couples battling infertility, that dream often hinges on the delicate science of in vitro fertilization (IVF). But what happens when those two lines don’t appear? When the hope turns into heartbreak?
IVF failure is a devastating reality for many couples, leaving them grappling with grief, anger, and a profound sense of loss. It’s a silent struggle, often shrouded in shame and secrecy. Yet, it’s far more common than you might think.
This comprehensive guide is here to shed light on the darkness of IVF failure. We’ll delve into the myriad causes, explore the emotional turmoil, and provide expert advice for coping and moving forward. We’ll uncover the hidden truths, answer your burning questions, and offer solace in knowing you’re not alone.
This isn’t just about medical procedures and statistics—it’s about the human experience. It’s about the raw emotions, the shattered dreams, and the unwavering resilience of those who dare to hope against hope. Whether you’re currently facing IVF failure or seeking to understand this complex issue, this guide is for you.
Let’s embark on this journey together, hand in hand, towards healing, hope, and ultimately, the family you long for.
Unmasking the Culprits: Delving into the Causes of IVF Failure
IVF isn’t a one-size-fits-all process. There are many interconnected factors that can influence its success. Understanding these factors is crucial for both patients and practitioners to make informed decisions and develop personalized treatment plans. Let’s unravel the mystery behind IVF failure, one piece at a time.
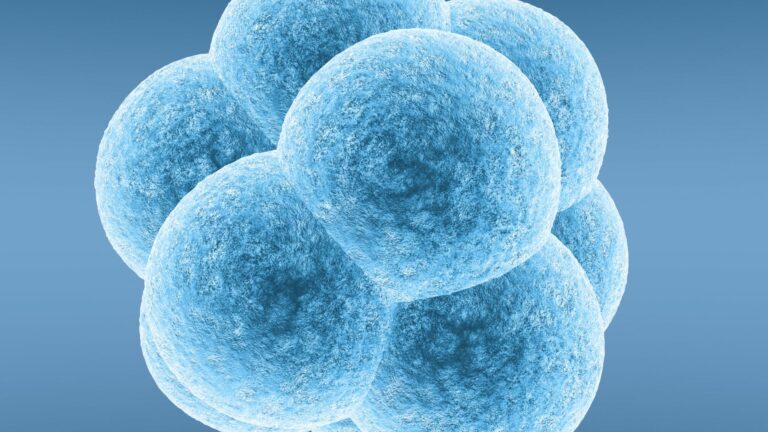
Egg-Related Factors: The Foundation of Life
The quality and quantity of a woman’s eggs play a pivotal role in IVF success. After all, these tiny cells hold the potential for new life.
Poor Egg Quality:
- Eggs can be affected by various factors, including age, genetics, and environmental toxins. These factors can lead to chromosomal abnormalities, impaired energy production, and other issues that hinder fertilization and embryo development.
- Diagnosing poor egg quality involves a combination of tests, such as antral follicle count (AFC), anti-Mullerian hormone (AMH) levels, and assessment of egg morphology during IVF. Treatment options may include using donor eggs, adjusting ovarian stimulation protocols, or utilizing specialized techniques like intracytoplasmic sperm injection (ICSI).
Diminished Ovarian Reserve:
- A woman’s ovarian reserve refers to the number and quality of eggs remaining in her ovaries. This reserve naturally declines with age, but it can also be affected by conditions like premature ovarian insufficiency (POI).
- Diminished ovarian reserve can lead to fewer eggs retrieved during IVF, lower fertilization rates, and poor embryo quality. Treatment options may include adjusting ovarian stimulation protocols, using donor eggs, or exploring alternative fertility treatments.
Genetic Abnormalities:
- Eggs can carry genetic abnormalities, such as aneuploidy (an abnormal number of chromosomes), which can prevent successful fertilization and embryo development.
- Preimplantation genetic testing (PGT-A) can help identify embryos with chromosomal abnormalities, allowing for the selection of healthy embryos for transfer. However, PGT-A is not without limitations and ethical considerations.
Sperm-Related Factors: The Other Half of the Equation
While often overlooked, sperm quality is just as important as egg quality for successful IVF.
Low Sperm Count or Motility:
- Low sperm count (oligospermia) and poor sperm motility (asthenospermia) can make it difficult for sperm to reach and fertilize an egg.
- Semen analysis is used to assess sperm count, motility, and morphology. Treatment options may include lifestyle changes, medication, or ICSI, where a single sperm is injected directly into an egg.
Abnormal Sperm Morphology:
- Abnormal sperm morphology (teratozoospermia) refers to sperm with abnormal shape or structure, which can affect their ability to fertilize an egg.
- Diagnosis involves microscopic examination of sperm. Treatment options may include ICSI, sperm selection techniques, or donor sperm.
Genetic Abnormalities:
- Similar to eggs, sperm can also carry genetic abnormalities that can affect fertilization and embryo development.
- PGT-M, a type of preimplantation genetic testing, can help identify sperm with genetic abnormalities, allowing for the selection of healthy sperm for ICSI. However, like PGT-A, PGT-M has limitations and ethical considerations.
Embryo-Related Factors: The Seeds of Potential
Even when fertilization occurs, a successful pregnancy is not guaranteed. The embryo itself can face challenges that hinder its development and implantation.
Poor Embryo Quality:
- Embryos are graded based on their appearance and developmental stage. Poor-quality embryos may have fragmentation, uneven cell division, or other abnormalities that compromise their viability.
- Advanced techniques like time-lapse imaging can help embryologists monitor embryo development and select the most promising ones for transfer. However, embryo grading isn’t foolproof and doesn’t guarantee success.
Genetic Abnormalities:
- Embryos can inherit genetic abnormalities from either parent, which can lead to miscarriage or developmental issues.
- PGT-A/PGT-M can be used to screen embryos for specific genetic conditions before transfer. However, these tests are not always recommended and can be costly.
Implantation Failure:
- Even a healthy embryo may fail to implant in the uterus. This can be due to various factors, including thin endometrial lining, immune system responses, or underlying health conditions.
- Tests like the endometrial receptivity array (ERA) and ReceptivaDx can assess the receptivity of the uterus and guide personalized treatment plans.
Uterine Factors: The Nurturing Environment
The uterus provides the environment for embryo implantation and growth. Any issues within the uterus can significantly impact IVF success.
Thin Endometrium:
- The endometrium is the lining of the uterus that thickens during the menstrual cycle to prepare for embryo implantation. A thin endometrium may not provide adequate support for the embryo.
- Measurement of endometrial thickness through ultrasound is crucial. Treatment options may include hormonal supplements, medication, or innovative therapies like platelet-rich plasma (PRP).
Uterine Abnormalities:
- Fibroids, polyps, or other structural abnormalities within the uterus can interfere with embryo implantation.
- Depending on their size and location, these abnormalities may require surgical removal before IVF.
Immune System Response:
- In some cases, the immune system may mistakenly attack the embryo as a foreign body, preventing implantation.
- Tests can assess immune system activity and guide immunotherapy treatments to improve implantation rates.
Other Factors: The Complex Web of Fertility
Fertility is a complex interplay of biological, environmental, and lifestyle factors.
Age-Related Decline in Fertility:
| Age Group | Live Birth Rate per IVF Cycle (Approximate) |
|---|---|
| Under 35 | 40-50% |
| 35-37 | 30-40% |
| 38-40 | 20-30% |
| Over 40 | 10-20% |
- A woman’s fertility naturally declines with age, primarily due to a decrease in egg quality and quantity. This decline accelerates after age 35.
- Older women may require more IVF cycles to achieve pregnancy, and the risk of miscarriage increases with age. Egg freezing at a younger age can preserve fertility for later use.
Underlying Health Conditions:
- Conditions like polycystic ovary syndrome (PCOS), endometriosis, and thyroid disorders can affect ovulation, hormone balance, and overall fertility.
- Managing these conditions with medication or surgery can improve IVF outcomes.
Lifestyle Factors:
- Obesity, smoking, excessive alcohol consumption, and chronic stress can negatively impact fertility.
- Adopting a healthy lifestyle can improve overall health and increase the chances of IVF success.
Unexplained Infertility:
- In some cases, the cause of infertility remains unknown despite extensive testing. This is known as unexplained infertility.
- Even with unexplained infertility, IVF can still be successful, but it may require a more empirical approach, trying different treatment protocols and adjusting them based on individual responses.
This exploration of the numerous factors contributing to IVF failure reveals the complexity of human reproduction.
Remember, each individual’s situation is unique, and the cause of IVF failure can be multifactorial. It’s crucial to consult with a fertility specialist for personalized evaluation and treatment.
Diagnosing the Roadblocks: Unraveling the Mystery of IVF Failure
Discovering why IVF fails isn’t always straightforward. It’s like solving a puzzle with multiple pieces, each contributing to the overall picture.
Monitoring During an IVF Cycle: Clues Along the Way
Throughout the IVF cycle, doctors closely monitor various parameters to assess how the body responds to treatment and gauge the progress of embryo development.
- Ultrasound: Used to track follicle growth in the ovaries and monitor endometrial thickness.
- Blood tests: Measure hormone levels (like estrogen and progesterone) to assess ovarian response and guide medication adjustments.
- Embryo assessments: Embryos are visually assessed for quality and developmental stage.
By carefully tracking these parameters, doctors can identify potential red flags early on and adjust the treatment plan as needed.
Post-Failure Evaluation: Piecing Together the Puzzle
After a failed IVF cycle, a thorough evaluation is crucial to uncover the underlying cause and optimize future treatment.
This evaluation may include:
- Review of previous cycle records: Analyzing medication dosages, hormone levels, and embryo quality.
- Additional testing:
- Genetic testing (PGT-A/PGT-M): To assess embryos for chromosomal abnormalities or specific genetic conditions.
- Tests for uterine receptivity: Such as the endometrial receptivity array (ERA) to determine the optimal window for embryo transfer.
- Tests for underlying health conditions: To rule out any contributing factors.
- Genetic testing (PGT-A/PGT-M): To assess embryos for chromosomal abnormalities or specific genetic conditions.
- Consultation with a fertility specialist: Discussing the findings, exploring potential explanations, and developing a revised treatment plan.
Genetic Testing: A Closer Look at the Genes
Preimplantation genetic testing (PGT-A/PGT-M) can provide valuable insights into the genetic health of embryos and help select the most viable ones for transfer. However, it’s important to understand the benefits and limitations of these tests:
Benefits:
- Increases the chances of successful implantation and live birth.
- Reduces the risk of miscarriage due to chromosomal abnormalities.
- Provides reassurance for couples with a family history of genetic conditions.
Limitations:
- Doesn’t guarantee a successful pregnancy.
- May result in fewer embryos available for transfer.
- Involves ethical considerations, particularly when discarding embryos with genetic abnormalities.
Seeking a Second Opinion: A Fresh Perspective
If a failed IVF cycle leaves you with unanswered questions or concerns, seeking a second opinion from another fertility specialist can be invaluable.
A fresh pair of eyes can:
- Re-evaluate your medical history and test results.
- Offer alternative interpretations or diagnoses.
- Suggest different treatment approaches or protocols.
Remember, you are your own best advocate. Don’t hesitate to seek multiple opinions and explore all available options to find the best path forward.
Navigating the Emotional Storm: Coping with Grief and Loss
IVF failure isn’t just a physical setback—it’s an emotional earthquake. The weight of dashed hopes and unfulfilled dreams can leave couples feeling lost, isolated, and overwhelmed.
Acknowledging the Emotional Impact: The Grief is Real
The grief that follows IVF failure is profound and multifaceted. It’s important to understand that this grief is valid and deserves to be acknowledged.
- Stages of Grief: It’s not uncommon to experience the classic stages of grief—denial, anger, bargaining, depression, and acceptance—but not necessarily in a linear fashion. You might cycle through these stages, experience them simultaneously, or skip some altogether.
- Feelings of Isolation: Many couples feel alone in their struggle, as infertility remains a taboo topic in many circles. This isolation can exacerbate feelings of sadness, shame, and inadequacy.
Building Resilience: Finding Strength in the Storm
While the pain of IVF failure is undeniable, there are ways to cope, heal, and emerge stronger on the other side.
- Therapy and Counseling: A mental health professional specializing in infertility can provide a safe space to process emotions, develop coping skills, and navigate the complexities of grief.
- Support Groups: Connecting with others who have experienced IVF failure can be incredibly empowering. Sharing experiences, offering support, and knowing you’re not alone can make a world of difference.
- Mind-Body Practices: Techniques like mindfulness, meditation, yoga, and acupuncture can help reduce stress, promote relaxation, and improve overall well-being.
Partner Communication: Strengthening Bonds Through Vulnerability
IVF failure can strain even the strongest relationships. Open and honest communication is essential for navigating this difficult time together.
- Open Dialogue: Talk to your partner about your feelings, fears, and hopes. Share your grief, anger, and disappointment without judgment or blame.
- Shared Grieving: Allow yourselves to grieve together, but also respect each other’s individual coping styles and needs.
- Relationship Support: Consider couples therapy to strengthen your bond, improve communication, and work through any challenges that may arise.
Self-Care Strategies: Nurturing Your Mind, Body, and Soul
During this challenging time, prioritizing self-care is crucial for your physical and emotional well-being.
- Mindfulness: Practice being present in the moment, focusing on your breath and bodily sensations.
- Journaling: Write down your thoughts and feelings to gain clarity and release pent-up emotions.
- Creative Outlets: Engage in activities that bring you joy and allow for self-expression, such as painting, writing, music, or spending time in nature.
Finding Meaning and Purpose: Redefining Your Journey
While IVF failure may feel like the end of a dream, it doesn’t have to be the end of your journey. Many couples find new meaning and purpose in the aftermath of loss.
- Volunteering: Giving back to others can be a powerful way to heal and find purpose. Consider volunteering for organizations that support infertility awareness or help families struggling with similar challenges.
- Advocacy: Sharing your story and advocating for infertility awareness can help break the silence and reduce stigma.
- Personal Growth: Use this experience as an opportunity for self-reflection, growth, and transformation. Explore new interests, hobbies, or career paths that bring you fulfillment.
Rebuilding Hope: What to Do After IVF Failure
The aftermath of IVF failure can feel like a desolate landscape. But amidst the disappointment, it’s crucial to remember that hope isn’t lost. There are avenues to explore, paths to consider, and a future to reclaim.
Discussing Options with Your Fertility Specialist: Charting the Next Course
The first step after a failed IVF cycle is to have a candid conversation with your fertility specialist. This isn’t about assigning blame, but rather about understanding what happened and exploring the best way forward.
During this discussion, you might:
- Review your previous cycle records: Analyze medication dosages, hormone levels, and embryo quality to pinpoint potential areas for improvement.
- Discuss further testing: Consider additional tests to assess uterine receptivity, genetic factors, or underlying health conditions that may have contributed to the failure.
- Explore treatment modifications: Depending on the findings, your doctor may suggest changes to the IVF protocol, such as different medications, timing adjustments, or alternative procedures like ICSI.
Considering Additional IVF Cycles: Weighing the Odds
For many couples, a single failed IVF cycle isn’t the end of the road. Multiple cycles may be necessary to achieve success.
- Success Rates: It’s important to understand that IVF success rates vary depending on numerous factors, including age, cause of infertility, and treatment protocol. While a single cycle may not yield the desired outcome, multiple cycles can significantly increase the cumulative success rate.
- Financial Implications: IVF is a significant financial investment. It’s crucial to discuss the cost of additional cycles, explore potential insurance coverage, and consider financial assistance programs if needed.
Exploring Alternative Paths to Parenthood: Beyond IVF
If additional IVF cycles aren’t feasible or desired, there are other avenues to explore on the path to parenthood.
- Adoption: Opening your heart and home to a child through adoption can be an incredibly fulfilling way to build a family. There are various types of adoption available, including domestic, international, and foster care adoption.
- Surrogacy: For women who are unable to carry a pregnancy, gestational surrogacy offers the opportunity to have a biological child. A gestational carrier carries the embryo created with the intended parents’ egg and sperm.
- Fostering: Becoming a foster parent provides a loving and stable home for children in need. While fostering may not lead to permanent adoption, it can be a rewarding way to make a positive impact on a child’s life.
Accepting Childlessness: Embracing a Different Path
For some couples, the path to parenthood may not involve having children of their own. While this can be a difficult realization, it’s important to acknowledge and embrace this possibility.
- Support Groups: Connecting with others who have chosen child-free living can provide support, understanding, and a sense of community.
- Counseling: Therapy can help couples grieve the loss of their dream of parenthood and explore alternative ways to find fulfillment and meaning in their lives.
- Life Planning: Re-evaluating goals, priorities, and aspirations can open up new possibilities for personal growth and happiness.
Preventing Future Heartache: Tips for Optimizing IVF Success
While IVF failure can feel like a setback, it doesn’t mean the door to parenthood is closed. There are proactive steps you can take to increase your chances of success in future cycles.
Lifestyle Modifications: Nurturing Your Body and Mind
Your lifestyle plays a significant role in your fertility. Making positive changes can optimize your overall health and improve your chances of conception.
- Diet: Focus on a balanced, nutrient-rich diet with plenty of fruits, vegetables, whole grains, and lean protein. Avoid processed foods, sugary drinks, and excessive caffeine.
- Exercise: Regular moderate exercise can help maintain a healthy weight, reduce stress, and improve blood flow to reproductive organs. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Stress Reduction: Chronic stress can negatively impact hormone levels and reproductive function. Explore stress-management techniques like yoga, meditation, deep breathing exercises, or spending time in nature.
- Supplements: Certain supplements like folic acid, CoQ10, and vitamin D may help improve egg and sperm quality. However, it’s important to consult with your doctor before starting any new supplements.
Preconception Health Optimization: Addressing Underlying Conditions
If you have any underlying health conditions, such as PCOS, endometriosis, thyroid disorders, or autoimmune diseases, it’s crucial to manage them effectively before and during IVF.
- Medication: Depending on the condition, your doctor may prescribe medication to regulate hormones, reduce inflammation, or address other underlying issues.
- Surgery: In some cases, surgery may be necessary to remove fibroids, polyps, or endometrial implants.
- Lifestyle changes: Adopting a healthy lifestyle, as discussed above, can also help manage chronic conditions and improve overall fertility.
Maximizing Egg and Sperm Quality: The Building Blocks of Life
The quality of eggs and sperm directly impacts the success of IVF. Several strategies can help optimize their health and viability.
- Supplements: Certain supplements, like CoQ10, vitamin D, and omega-3 fatty acids, have shown potential for improving egg and sperm quality.
- Medications: In some cases, medications may be prescribed to stimulate egg production, improve sperm motility, or enhance overall reproductive function.
- Lifestyle changes: Adopting a healthy lifestyle, including maintaining a healthy weight, avoiding smoking and excessive alcohol, and managing stress, can significantly improve egg and sperm quality.
Preimplantation Genetic Testing (PGT-A/PGT-M): A Window into Embryo Health
PGT-A and PGT-M allow for the genetic screening of embryos before transfer. While these tests can increase the chances of a healthy pregnancy, they’re not always recommended and should be discussed thoroughly with your doctor.
- Who should consider PGT?
- Couples with a family history of genetic disorders.
- Women over 35, as the risk of chromosomal abnormalities in embryos increases with age.
- Couples who have experienced recurrent miscarriages.
- Pros and Cons: PGT can offer valuable information, but it’s important to weigh the potential benefits against the cost, invasiveness, and ethical considerations.
Choosing the Right Clinic and Doctor: Your Partners in the Journey
The clinic and doctor you choose can significantly impact your IVF experience and outcome.
- Experience and Success Rates: Research clinics and doctors with proven experience and success rates in treating your specific type of infertility.
- Communication and Support: Choose a clinic and doctor who listen to your concerns, answer your questions, and provide emotional support throughout the process.
- Personalized Approach: Look for a clinic that tailors treatment plans to your individual needs and circumstances, rather than relying on a one-size-fits-all approach.
Realistic Expectations: Managing Hope and Disappointment
While it’s important to maintain hope, it’s equally important to have realistic expectations about IVF.
- Understand the Statistics: IVF success rates vary widely depending on numerous factors. Your doctor can provide a personalized assessment based on your individual circumstances.
- Focus on the Process: While the ultimate goal is a healthy baby, focus on each step of the IVF process and celebrate small victories along the way.
- Seek Support: Don’t hesitate to seek emotional support from friends, family, therapists, or support groups to help manage the emotional rollercoaster of IVF.
By taking proactive steps and adopting a holistic approach, you can maximize your chances of IVF success and overcome the challenges of infertility.
The Financial Burden: Navigating the Cost of IVF Failure
The emotional toll of IVF failure is undeniable, but the financial strain can be equally overwhelming. IVF is a significant investment, and repeated failed cycles can quickly drain resources.
Breakdown of IVF Costs: A Closer Look at the Expenses
- Medications: Fertility drugs used for ovarian stimulation can be expensive, costing thousands of dollars per cycle.
- Procedures: Egg retrieval, sperm preparation, embryo culture, and embryo transfer all come with their own price tags.
- Testing: Diagnostic tests like ultrasounds, blood work, and genetic testing can add up quickly.
- Additional Treatments: In some cases, additional treatments like ICSI or PGT-A/PGT-M may be recommended, increasing the overall cost.
Insurance Coverage: A Patchwork of Policies
Insurance coverage for IVF varies widely depending on your state and insurance provider.
- State Mandates: Some states have mandated coverage for IVF, while others offer limited or no coverage.
- Insurance Policies: Even with mandated coverage, policies may have restrictions on the number of cycles covered, age limits, or specific diagnoses required for eligibility.
- Advocacy: Organizations like RESOLVE provide resources and advocacy tools to help navigate insurance coverage for fertility treatments.
Financial Assistance Programs: A Ray of Hope
For many couples, the financial burden of IVF can feel insurmountable. However, there are resources available to help.
- Grants: Non-profit organizations like the Cade Foundation offer grants to help cover the cost of fertility treatments.
- Loans: Specialized fertility financing companies offer loans with lower interest rates and flexible repayment terms.
- Discounts: Some clinics and pharmacies offer discounts or payment plans to make IVF more affordable.
- Clinical Trials: Participating in clinical trials can provide access to cutting-edge treatments at a reduced cost.
Budgeting and Financial Planning: Taking Control of Your Finances
Careful financial planning is essential when undergoing IVF.
- Set a budget: Determine how much you’re willing and able to spend on fertility treatments.
- Track expenses: Keep detailed records of all IVF-related costs.
- Explore financing options: Research grants, loans, and discounts that may be available to you.
- Communicate with your clinic: Discuss financial concerns with your clinic’s financial counselor to explore payment options and create a manageable plan.
While the financial burden of IVF failure can be significant, it’s important to remember that there are resources available to help.
With careful planning and support, you can navigate the financial challenges and focus on your journey toward parenthood.
Your Journey Continues: Finding Hope After IVF Failure
The road to parenthood isn’t always a straight line. It can be filled with twists, turns, and unexpected detours. IVF failure is one of those detours—a painful one, no doubt—but it doesn’t have to be the end of your journey.
Recap of Key Takeaways: What We’ve Learned
- IVF failure is a common experience, affecting many couples worldwide.
- It can be caused by a multitude of factors, including egg and sperm quality, embryo health, uterine conditions, and underlying medical issues.
- Diagnosing the cause of failure requires a comprehensive evaluation, including reviewing medical history, conducting additional tests, and seeking expert opinions.
- The emotional impact of IVF failure is significant, and coping strategies such as therapy, support groups, and self-care are essential for healing.
- There are various options to consider after a failed IVF cycle, including further IVF attempts, alternative fertility treatments, adoption, surrogacy, or choosing a child-free life.
- By understanding the causes, seeking appropriate treatment, and adopting a healthy lifestyle, you can optimize your chances of IVF success in the future.
Emphasis on Hope and Resilience: Your Story Isn’t Over
While IVF failure can feel like a devastating blow, it’s important to remember that there is always hope. Many couples who face setbacks go on to have successful pregnancies, either through IVF or other avenues.
Your journey may take longer and involve more challenges than you initially anticipated, but it’s a journey worth taking.
Encouraging Further Research and Support: Knowledge is Power
The field of reproductive medicine is constantly evolving, with new research and treatments emerging regularly. Staying informed about the latest advancements can empower you to make informed decisions about your fertility journey.
Here are some resources to help you stay informed and connected:
- National Infertility Association (RESOLVE): A non-profit organization providing support, education, and advocacy for individuals and families facing infertility.
- American Society for Reproductive Medicine (ASRM): A professional organization for reproductive medicine specialists, offering patient resources and information on the latest research and treatments.
- Support Groups: Local and online support groups provide a safe space to connect with others who understand the challenges of infertility and IVF failure.
Remember, you are not alone in this journey. Millions of couples worldwide face infertility, and countless others have experienced the heartache of IVF failure. By seeking support, staying informed, and remaining hopeful, you can navigate this challenging path and find your own unique way to build the family you desire.
Certainly. I’ll create a new section that seamlessly blends with the article and explains the relationships between the internal links and the main topic of IVF failure. Here’s the new section:
Understanding the Bigger Picture: Related Topics in IVF
As we navigate the complex journey of IVF failure, it’s important to understand how various aspects of IVF are interconnected. Let’s explore some related topics that can provide a more comprehensive understanding of the IVF process and its challenges.
IVF Success Rates
Understanding IVF success rates is crucial when dealing with IVF failure. These rates can vary widely based on factors such as age, underlying fertility issues, and treatment protocols. By examining success rates, you can gain realistic expectations and better contextualize your own experience with IVF failure.
Strategies to Increase IVF Success Chances
After experiencing an IVF failure, many couples seek ways to improve their chances in future cycles. This resource provides valuable insights into lifestyle changes, medical interventions, and advanced techniques that can potentially boost IVF success rates, offering hope and actionable steps for those who have faced setbacks.
Preimplantation Genetic Screening
Genetic factors can play a significant role in IVF failure. Preimplantation genetic screening (PGS) is a technique used to identify chromosomal abnormalities in embryos before transfer. Understanding PGS can help you make informed decisions about whether this additional step might be beneficial in preventing future IVF failures.
IVF Cost in India
The financial aspect of IVF is an important consideration, especially when dealing with failed cycles. This resource provides information on IVF costs in India, helping you plan for potential future treatments and understand the financial implications of multiple IVF attempts.
IVF Financial Burden
Failed IVF cycles can compound the already significant financial stress associated with fertility treatments. This topic explores the financial burden of IVF, offering insights into managing costs, exploring financial assistance options, and coping with the economic impact of multiple cycles.
IVF Protocols for Diminished Ovarian Reserve
Diminished ovarian reserve can be a contributing factor to IVF failure. Understanding specialized protocols for this condition can be crucial for those who have experienced failed cycles due to poor egg quality or quantity.
Chromosomal Abnormalities and Karyotyping in IVF
Chromosomal abnormalities are a common cause of IVF failure and recurrent miscarriages. Karyotyping is a technique used to detect these abnormalities. Learning about this process can help you understand potential genetic factors contributing to IVF failure and explore options for genetic testing.
Intracytoplasmic Sperm Injection (ICSI)
ICSI is an advanced technique used in IVF to overcome certain male factor infertility issues. For couples who have experienced IVF failure due to fertilization problems, understanding ICSI can provide insight into a potential solution for future cycles.
By exploring these related topics, you can gain a more comprehensive understanding of the factors influencing IVF outcomes. This knowledge can empower you to make informed decisions, have more productive conversations with your healthcare providers, and navigate the challenging journey of IVF with greater confidence and hope.